Core Services

1 Initial Consultation and Diagnostic Testing
Comprehensive medical history review
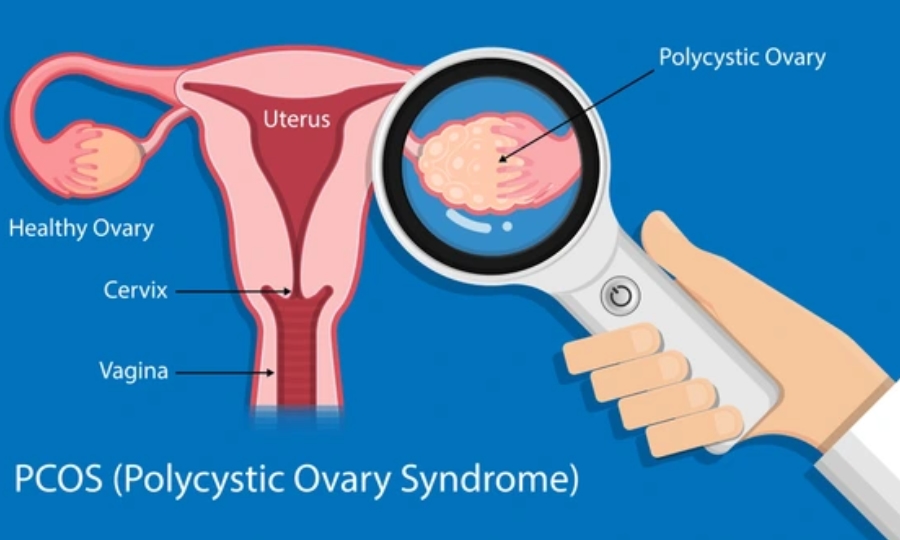
Blood tests, ultrasounds, and other diagnostic procedures
Personalized treatment planning

2 Ovarian Stimulation and Monitoring
Hormonal medications to stimulate egg production
Regular monitoring through blood tests and ultrasounds

3- Egg Retrieval and Sperm Collection
Minor surgical procedure to collect eggs
Collection and processing of sperm samples

4-Fertilization and Embryo Culture
Conventional IVF and ICSI (Intracytoplasmic Sperm Injection)
Embryo culture and monitoring in a controlled lab environment

5-Embryo Transfer
Transfer of one or more embryos into the uterus
Luteal phase support with hormonal medications

6-Pregnancy Testing and Follow-Up
Blood tests to confirm pregnancy
Follow-up appointments and ultrasounds to monitor early pregnancy

7-Advanced Reproductive Technologies
Advanced Reproductive Technologies
Embryo culture and monitoring in a controlled lab environment

8-Emotional and Psychological Support
Counseling services for emotional support
Support groups and community resources

9-Financial Guidance
Detailed cost breakdown and financial planning
Assistance with insurance coverage and financing options
Computerized Semen Analysis and Sperm Class Analyzer (SCA)
Computer-Assisted Semen Analysis (CASA) systems are advanced tools used in IVF clinics to provide objective and precise evaluations of semen samples. These systems use specialized software and imaging technology to analyze various parameters of sperm quality.
Key Features:
Sperm Concentration:
Measures the number of sperm cells per milliliter of semen.
Motility Assesses the percentage of moving sperm and categorizes their movement patterns (e.g., rapid, slow, non-progressive).
Morphology: Evaluates the shape and structure of sperm cells to identify abnormalities.
Vitality: Determines the percentage of live sperm in the sample.
DNA/ Fragmentation:
Analyzes the integrity of sperm DNA, which is crucial for successful fertiliz
Benefits:
Accuracy and Consistency: Provides more reliable results compared to manual analysis.
Efficiency: Faster processing and analysis of samples.
Standardization: Reduces variability in results, ensuring consistent quality of analysis.
Sperm Class Analyzer (SCA):
The Sperm Class Analyzer (SCA) is a specific type of CASA system that offers comprehensive analysis of semen samples. It is widely used in both human and animal fertility clinics.
Key Features:
Modular Software: Allows for the analysis of various parameters, including concentration, motility, morphology, DNA fragmentation, vitality, and acrosome reaction.
Automated Analysis: Uses high-resolution cameras and advanced algorithms to analyze sperm samples.
User-Friendly Interface: Provides easy-to-use software with detailed reporting and visualization options(https://www.micropticsl.com/products/sperm-class-analyzer-casa-system/).
Applications:

Fertility Assessment
Helps in diagnosing male infertility by providing detailed sperm analysis.

Treatment Monitoring
Tracks changes in sperm quality over time, which is useful for evaluating the effectiveness of treatments.
These advanced tools are essential in IVF clinics for providing accurate and detailed assessments of sperm quality, which is crucial for diagnosing infertility and planning effective treatments.
Comprehensive Initial Consultation

Medical History Review:
Detailed discussion of the patient’s medical history, previous fertility treatments, and any underlying health conditions.

Diagnostic Tests:
Blood tests, ultrasound scans, and other diagnostic procedures to assess ovarian reserve, uterine health, and sperm quality.

Personalized Treatment Plan:
Based on the results, a tailored treatment plan is developed, including medication protocols and timelines.
2-Ovarian Stimulation and Monitoring

Medications.
Hormonal injections (e.g., FSH, LH) are administered to stimulate the ovaries to produce multiple eggs. The dosage and duration are customized for each patient.
Monitoring.
Regular blood tests and ultrasounds monitor the development of follicles (egg-containing sacs) in the ovaries. Adjustments to medication may be made based on the response.
3-Egg Retrieval Procedure

Preparation:
Before the procedure, a trigger shot (hCG) is given to mature the eggs.

Procedure:
Under sedation, a thin needle is guided through the vaginal wall to the ovaries to aspirate the eggs. This is done using ultrasound guidance and typically takes about 20-30 minutes.

Recovery:
Patients may experience mild cramping or spotting but can usually resume normal activities the next day.
4- Fertilization and Embryo Culture
Sperm Collection: A sperm sample is collected from the partner.
Fertilization Methods:
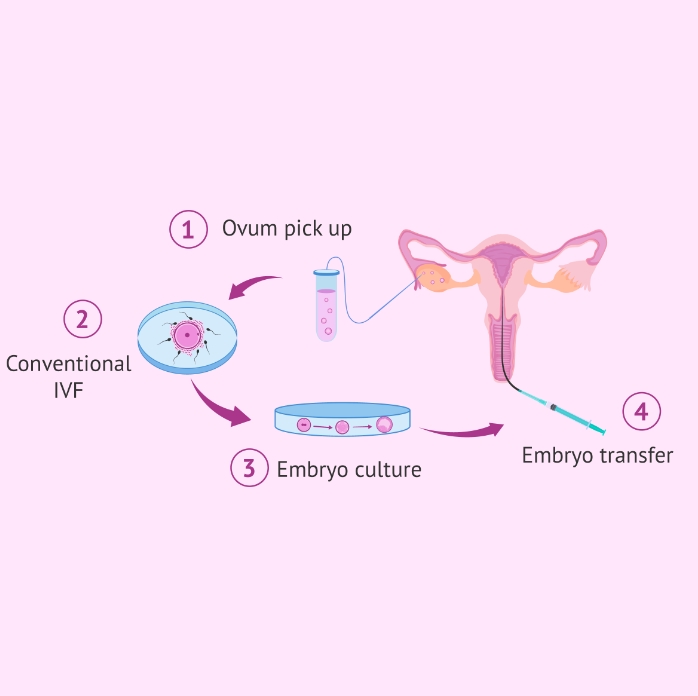
Conventional IVF:
Eggs and sperm are mixed together in a petri dish and left to fertilize naturally.
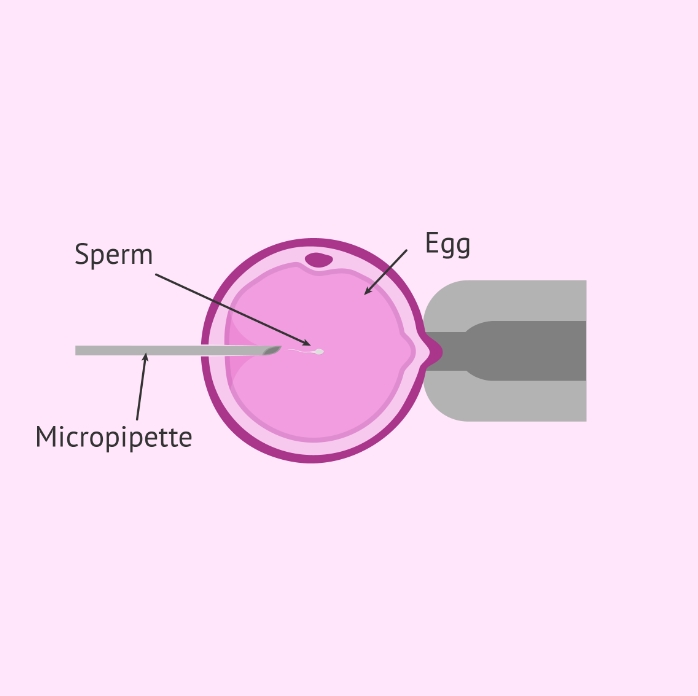
ICSI (Intracytoplasmic Sperm Injection):
A single sperm is injected directly into an egg, often used in cases of male infertility.
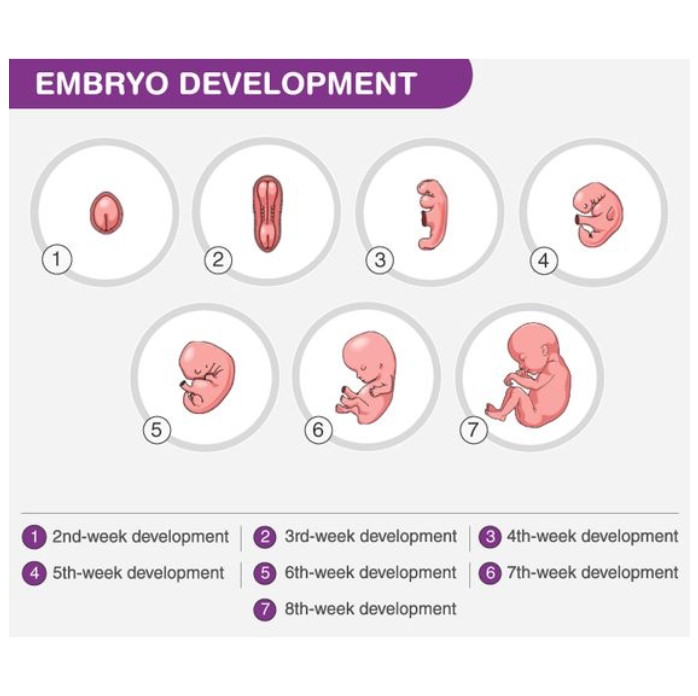
Embryo Culture:
Fertilized eggs (embryos) are cultured in a controlled environment for 3-5 days until they reach the blastocyst stage. Embryologists monitor their development and select the best quality embryos for transfer.
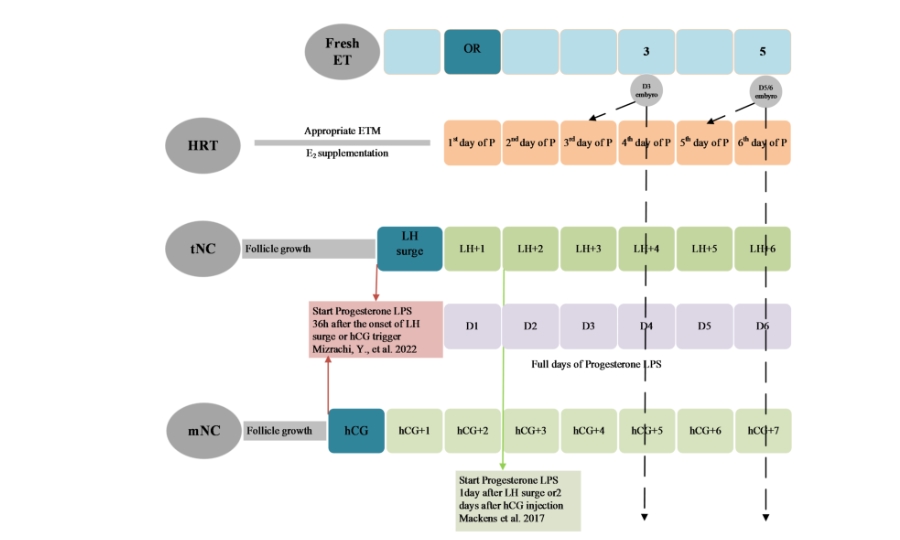
5- Embryo Transfer and Luteal Phase Support
Embryo Transfer
One or more embryos are transferred into the uterus using a thin catheter. This procedure is quick and usually painless.
Luteal Phase Support:
Hormonal support (e.g., progesterone) is provided to help maintain the uterine lining and support early pregnancy.
6- Pregnancy Test and Follow-Up
Pregnancy Test:
About 10-14 days after the embryo transfer, a blood test is conducted to check for pregnancy.
Follow-Up:
If the test is positive, follow-up ultrasounds and appointments are scheduled to monitor the pregnancy. If negative, the clinic will discuss next steps and potential adjustments for future cycles.
7-Advanced Techniques and Options

Cryopreservation:
Excess embryos can be frozen for future use, allowing for additional attempts without repeating the entire IVF cycle.
General Structure, Instruments, and Medical Equipment in the AFC Clinic

Reception and Waiting Area
-Welcoming environment for patients and visitors.
-Comfortable seating, informational brochures, and patient support resources.Personalized treatment planning

Laboratory
Embryology Lab : Sterile environment where eggs and sperm are handled, fertilization occurs, and embryos are cultured.
Andrology Lab: Area dedicated to sperm analysis and processing.
Cryopreservation Lab Facilities for freezing and storing eggs, sperm, and embryos.
General blood work lab

Procedure Rooms
Egg Retrieval Theater: Equipped for minor surgical procedures to retrieve eggs.
Embryo Transfer Room: Comfortable and sterile environment for transferring embryos into the uterus.
Instruments and Medical Equipment

Ultrasound Machines
Used for monitoring ovarian follicles, guiding egg retrieval, and assessing uterine lining.
Instruments and Medical Equipment.

Ultrasound Machines
Used for monitoring ovarian follicles, guiding egg retrieval, and assessing uterine lining.

Surgical Instruments
Needles and Catheters: Used for egg retrieval and embryo transfer.
Aspiration Pumps: Assist in the retrieval of eggs from the ovaries.

Incubators
Maintain optimal conditions for embryo culture, including temperature, humidity, and gas composition.

Microscopes
High-powered microscopes for examining eggs, sperm, and embryos.
Embryo culture and monitoring in a controlled lab environment

Centrifuges
Used in the andrology lab to process and separate sperm samples.

Cryopreservation Equipment
Counseling services for emotional support
Support groups and community resources

Laminar Flow Hoods
Provide a sterile environment for handling gametes and embryos, protecting them from contamination.

Hormonal Medications
Blood Test Analyzers: Measure hormone levels and other important markers.Stimulate the ovaries to produce multiple eggs.
Genetic Testing Equipment: Used for Preimplantation Genetic Testing (PGT) to screen embryos for genetic abnormalities.

Monitoring and Diagnostic Tools
Gonadotropins: Stimulate the ovaries to produce multiple eggs.
Progesterone: Supports the uterine lining and early pregnancy.
Surgical Instruments

Needles and Catheters:
Used for egg retrieval and embryo transfer.
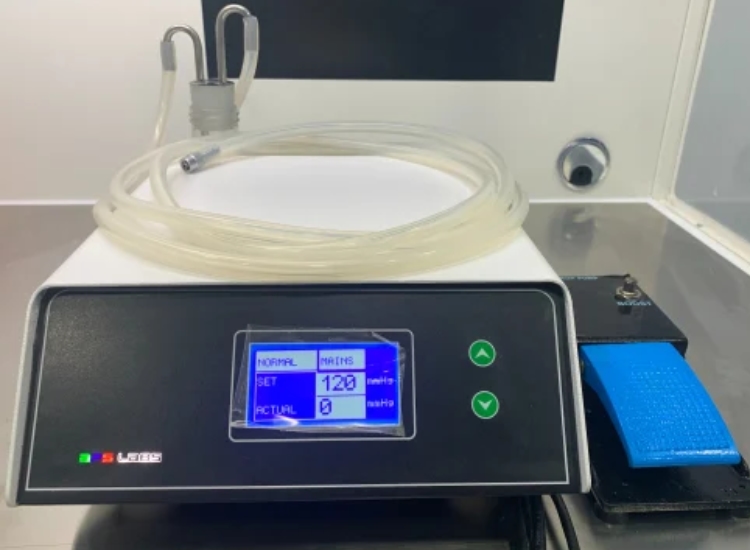
Aspiration Pumps:
Assist in the retrieval of eggs from the ovaries.
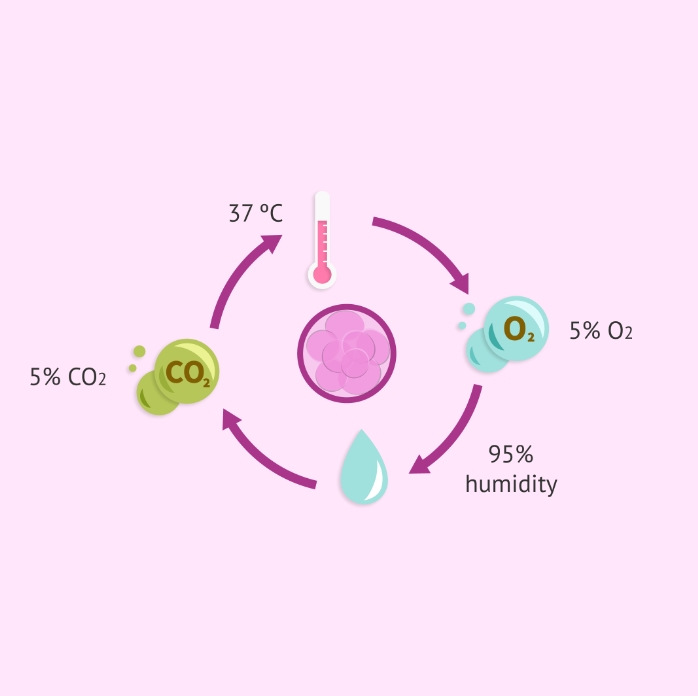
CO2 Incubators in IVF Clinics :
Purpose and Function
CO2 incubators are essential in IVF clinics for creating and maintaining the optimal environment needed for the growth and development of embryos. These incubators precisely control temperature, humidity, and CO2 levels to mimic the conditions of the human body, ensuring the best possible outcomes for embryo culture.
Key Features :-

Temperature Control
Maintains a stable temperature, typically around 37°C, which is crucial for embryo development.
CO2 Regulation
CO2 levels are kept at around 5-6% to maintain the correct pH in the culture media, which is vital for cell growth and embryo development.

Humidity Control
High humidity levels (95% or higher) are maintained to prevent the culture media from evaporating and to ensure a stable environment.

Sterility and Contamination Control:
Equipped with HEPA filters and UV sterilization to minimize the risk of contamination.
Some models have copper interiors to reduce microbial growth.

Alarm Systems:
Built-in alarms to alert staff of any deviations from set parameters, ensuring immediate corrective action can be taken.

Eautomated Sterilization Cycles:
High-temperature decontamination cycles that can be scheduled to ensure a sterile environment.
X-Ray Diagnosis: Hysterosalpingography (HSG)
Hysterosalpingography (HSG) is an X-ray procedure used to evaluate the condition of the uterus and fallopian tubes. It is particularly useful in diagnosing issues related to infertility.
Procedure:
Preparation
The procedure is scheduled after menstruation but before ovulation to ensure the patient is not pregnant.

Contrast Dye:
A contrast dye is injected into the uterine cavity through the cervix.

X-Ray Imaging:
X-ray images are taken as the dye flows through the uterus and fallopian tubes. This helps to visualize any blockages or abnormalities.
Uses:

Blocked Fallopian Tubes:
Identifies blockages that could prevent sperm from reaching the egg.
Uterine Abnormalities:
Detects structural issues such as fibroids, polyps, or congenital anomalies.

Post-Surgical Evaluation:
Checks the success of procedures like tubal ligation or reversal.
Better Diagnostic Accuracy: Provides more detailed and accurate information about fetal development and potential issues compared to standard 2D ultrasounds.
Benefits and Considerations
Diagnostic Accuracy:Provides detailed images and direct visualization, leading to accurate diagnoses.
Combined Procedures: Hysteroscopy can be both diagnostic and therapeutic, reducing the need for multiple procedures.
3D and 4D Sonography in IVF Clinics
Overview
3D and 4D sonography are advanced ultrasound techniques used in IVF clinics to provide detailed images and videos of the developing fetus. These technologies enhance the ability to monitor fetal development and diagnose potential issues.

3D Sonography
Definition: 3D sonography creates three-dimensional images of the fetus by compiling multiple two-dimensional images taken from different angles.

Contrast Dye:
A contrast dye is injected into the uterine cavity through the cervix.

X-Ray Imaging:
X-ray images are taken as the dye flows through the uterus and fallopian tubes. This helps to visualize any blockages or abnormalities.
4D Sonography
Definition:
4D sonography adds the dimension of time to 3D images, creating live video footage of the fetus in motion.
Uses:

Real-Time Monitoring:
Allows parents and doctors to see the fetus move, yawn, stretch, or even smile in real-time.

Enhanced Diagnosis:
Provides dynamic views of fetal movements and behaviors, which can be useful in assessing fetal health

Procedure:
Similar to 3D sonography, but the images are continuously updated to create a video effect.
-
CONTACT INFO
-
Contact us
Benghazi - Libya
info@alamalfertility.ly
218 91 0433 000